Retina
The retina is a thin, fragile layer of nervous tissue that lines the back of the eye on the inside.
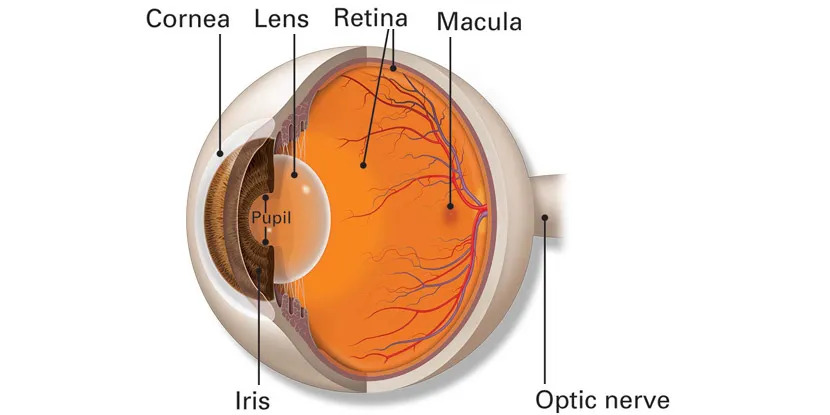
The cornea and lens focus the light onto the retina. The photoreceptors cells in the retina convert the focused light rays into chemical signals and send those to the visual centres of the brain through the optic nerve.
Retina is differentiated into 10 layers
- Pigment epithelium.
- Layer of rods and cones
- External limiting membrane
- Outer nuclear layer
- Outer plexiform layer
- Inner nuclear layer
- Inner plexiform layer
- Ganglion cell layer
- Nerve fibre layer
- Internal limiting membrane
Things to note about Retina
The major regions of the retina are the Optic disc, Retinal blood vessels, Area centralis with the fovea and foveola, Peripheral retina and the ora serrata.
-
Optic Disc: The retina is thickest near the optic disc. It becomes thinner towards the periphery. The optic disc is a circular to somewhat oval in structure that measures approximately 1.5 mm in diameter. Centrally, it contains a depression which is known as the physiological cup.
-
Central Retina: The area central retina is distinguishable into the fovea and foveola. The fovea is the approximate centre of the central retina. The foveola is the area of the highest visual acuity in the retina.
-
Macula Lutea: The macula lutea is an oval zone of yellow colouration in the posterior retina. The light rays coming from the objects we see are focussed sharply on forea in the central retina which is situated in the macula. Hence, it is responsible for sharp and central vision.
-
Peripheral Retina: It increases the field of vision. When we are looking straight at an object without moving our eyes and head, we can also see a few objects / things adjacent to the object of our focus. It is because of peripheral vision and the peripheral retina is responsible for it.
The Most common retinal problems observed are:
- Diabetic Retinopathy
- Age Related Macular Degeneration
- Retinal vein and artery occlusion disorders
- Central Serous Retinopathy
- Retinal Detachment
- Hypertensive Retinopathy
- Macular Oedema, etc.,
Among these the most common Retinal Problem is Diabetic Retinopathy
Diabetic Retinopathy:
It refers to retinal changes seen in patients with Diabetes mellitus. With increase in the life expectancy of diabetics, the incidence of diabetic retinopathy (DR) has increased.
The prevalence of diabetic retinopathy (DR) is about 4 to 28%, and about 2% of diabetic population is blind as a result of this disease. The best predictor of diabetic retinopathy is the duration of diabetes.
The severity of the diabetic retinopathy, generally parallels the duration of the disease and the adequacy of its control, and not the severity of the diabetes. The course and severity of Diabetic Retinopathy are affected by the presence of nephropathy, systemic hypertension, pregnancy, and positive family history.
Know the risk Factors for Diabetic Retinopathy:
- Duration of diabetes is the most important determining factor.
- Poor metabolic control is less important than duration, but is nevertheless relevant to the development and progression of DR.
- The effect of heredity is more on the proliferative retinopathy.
- Pregnancy may accelerate the changes of diabetic retinopathy.
- Hypertension, when associated, may also accelerate the changes of diabetic retinopathy.
- Other risk factors include smoking, consumption of alcohol, obesity. .
- During the early stages of diabetic retinopathy, some of the patients may not notice any change in their vision and therefore it is very important for the patient to consult an ophthalmologist periodically for the evaluation of their retina.
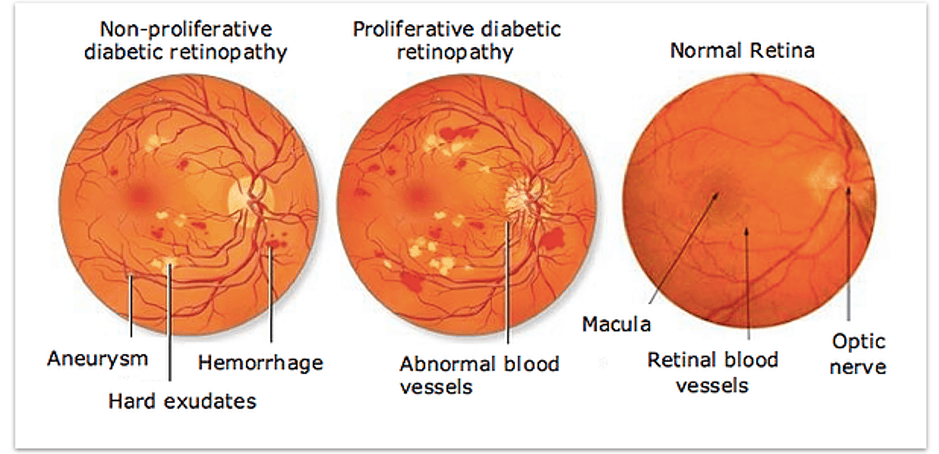
Diabetic Retinopathy is of two types:
Non-proliferative diabetic retinopathy:
Non-proliferative diabetic retinopathy (NPDR) is the beginning phase of the disease where the symptoms will be mild or non-existent. In NPDR, the vessels in the retina are affected and may release fluid into the retina. This spillage may promote swelling of the macular area.
Proliferative diabetic retinopathy:
In Proliferative diabetic retinopathy, new blood vessels grow over the surface of the Retina and also into the Vitreous. Since they are fragile, they easily rupture and leak blood into the Vitreous cavity.
Complications:
- Vitreous Haemorrhage
- Retinal Detachment
- Neovascular Glaucoma
Diagnosing Diabetic Retinopathy:
After the primary workup done by the optometrist (which include complete history taking, measuring visual acuity, refraction, slit-lamp examination and IOP measuring), dilating drops will be instilled in patient’s eyes to widen the pupil.
Ophthalmologists evaluate the retina with the help of Indirect ophthalmoscope and slit lamp biomicroscope. After a thorough examination of the retina if the patient is diagnosed to have Diabetic Retinopathy, then the patient may be asked to go for a few tests like FFA (Fundus Fluorescein Angiography) and OCT (Optical Coherence Tomography).
Symptoms:
- Blurring of vision
- appearance of floaters
- observing dark areas in your field of vision
- loss of vision
How our experts at Sri Krishna Eye Institute diagnose Diabetic Retinopathy:
Our team of ophthalmologists and optometrists perform a comprehensive eye examination on the patient’s eyes. We do a complete and detailed history taking of the patients, visual acuity testing, objective refraction followed by subjective refraction to know if there is a need to change your spectacle prescription, slit lamp evaluation, applanation tonometry for intraocular pressure, dilatation(to widen the pupil) followed by our team of ophthalmologists for the evaluation of the retina with Indirect Opthalmoscope. Then the patient may be asked to go for a few tests like FFA (Fundus Fluorescein Angiography) and OCT (Optical Coherence Tomography).
At Sri Krishna Eye Institute, we have got some of the most advanced equipment for the Diagnosis and Treatment of Retinal Diseases.
-
Carl Zeiss 532S Green Laser for Laser treatment.
-
Bausch & Lomb Stellaris PC for Vitrectomy Surgeries. The first installation was done at Sri Krishna Eye Institute in the entire Coastal Andhra.
-
Carl Zeiss VISU 200 Microscope with BIOM for Vitrectomy Surgeries. This was first installed in
Sri Krishna Eye Institute in the entire Coastal Andhra.
.jpeg)
Management of Diabetic Retinopathy:
To prevent visual loss occurring from diabetic retinopathy a periodic follow-up is very important for a timely intervention.
Strict metabolic control of blood sugar, Lipid reduction, Control of associated anaemia, and Control of other associated systemic diseases.
The various treatments for Diabetic Retinopathy are:
-
Laser Treatment:
-
Intra-vitreal Anti VEGF Injection:
-
Vitrectomy Surgery
All the above mentioned modalities of treatment are available at Sri Krishna Eye Institute
